The Growing Concern: Is Polycystic Ovary Syndrome (PCOS) Really Becoming More Common?
Are Polycystic Ovary Syndrome (PCOS) cases really on the rise, or is our awareness and understanding of the condition only improving?
PCOS, a hormonal disorder causing enlarged ovaries with small cysts, is widely known to affect 1 in 10 women of reproductive age. However, recent headlines suggest these figures are rising. This article will take a deep dive into what PCOS truly is, why it's perceived to be increasing, and whether this perspective holds any truth. We’ll also look into the symptoms, which can often go unnoticed, and finally, explore how we heal, recover and treat PCOS. So, whether you're a patient, a keen learner, or simply curious, join us as we unravel the complexities of PCOS.
Unmasking PCOS: The Hidden Hormonal Disruptor
Polycystic Ovary Syndrome, or PCOS, is a common endocrine disorder that often afflicts women during their reproductive years. It's characterised by the presence of small, fluid-filled sacs—or cysts—on the ovaries, which, as the name suggests, gives this condition its distinctive label. But PCOS is more than just an ovarian issue: it's a comprehensive metabolic disorder throwing a spanner in the works of your hormonal system.
Women with this condition often face an overproduction of insulin and androgens, which are male hormones, leading to wide-ranging symptoms such as irregular menstrual cycles, excessive hair growth, acne, and even obesity. This hormonal chaos inside the body also increases the risk of reproductive, cardiovascular, and metabolic health issues.
Throughout the years, the medical community has continuously expanded its understanding of PCOS, but the condition, often presented with confusing and overlapping symptoms, remains shrouded in mystery.
How to know if you might have PCOS
Now you may be asking, "how would I know if I have PCOS?"
PCOS symptoms can sometimes be subtle or mistaken for other things. But there are a few common signs to be aware of.
One common sign is irregular periods, which means they might come at different times each month or you might miss them altogether. Having fewer than eight periods in a year is a typical indicator.
Some women with PCOS may also experience increased hair growth on their face or body. This is called hirsutism and affects about 70% of women with PCOS. You might also find it harder to lose weight or experience weight gain, even if you haven't changed your diet or exercise routine.
Skin concerns are another possible symptom. Acne breakouts are common for many women, and PCOS can contribute to them. You might also notice darker patches of skin on your neck, groin, or under your breasts.
It's important to remember that many women with PCOS haven't been diagnosed yet - one study found that a staggering 50-70% of women with PCOS are yet to be diagnosed!
So if you're experiencing any of these signs, it's a good idea to talk to your doctor to learn more about PCOS and discuss if testing might be right for you.
how is PCOS treated?
Have you ever wondered how Polycystic Ovary Syndrome (PCOS) is actually treated? If you or someone you know has been diagnosed with this condition, understanding the range of treatment options can be crucial, and thankfully there are numerous strategies to manage it.
First and foremost, it's important to remember that the approach to treating PCOS is generally individualised, usually depending on the patient's symptoms and goals, such as reducing the risk of complications, managing the symptoms or preparing for pregnancy. This reframes the disease management into a highly personalised treatment experience, with each patient receiving unique advice and treatment options.
According to the American College of Obstetricians and Gynecologists, lifestyle modification is often the first line of therapy for women with PCOS. Studies indicate that weight loss of as little as 5 percent can improve insulin sensitivity, menstrual regularity, and fertility, while decreasing the risk of developing diabetes. Diet and exercise play a crucial role in managing PCOS, with a focus on a balanced diet and regular physical activity.
If lifestyle changes alone are not sufficient, medications can be prescribed to manage specific symptoms. Birth control pills, for instance, can regulate menstrual cycles and reduce levels of male hormones, which, in turn, can help control acne and excess hair growth. Other medicines like Metformin can improve insulin resistance, which can be particularly beneficial for patients with PCOS.
A smaller subset of patients may opt for procedures such as fertility treatments or surgery if they're experiencing fertility issues and other treatments haven’t been successful. Procedures like laparoscopic ovarian drilling (LOD) or in vitro fertilization (IVF) may be recommended.
why is it so hard to get diagnosed with pcos?
PCOS often goes unnoticed due to overlapping symptoms with other gynaecological issues. Dr. Grover highlights “Insulin resistance and chronic inflammation often present with other ailments that are also debilitating and are also worked up first,”.
Dr. Cree, MD, PhD, an associate professor of pediatric endocrinology at the University of Colorado and the director of the PCOS Multi-Disciplinary Clinic shares that “many females who do have irregular periods and are not trying to get pregnant are offered a combined oral contraceptive or other similar hormone treatment to fix the timing of periods without a [blood] workup,”
Clear diagnostic guidelines emerged in 2018, yet many providers lag behind. Patients must raise concerns about irregular menstruation and related changes to prompt necessary testing. Pollie cofounder Jane Sagui emphasises the simplicity of diagnostic tests—hormone levels and ultrasounds—advising patients to request these specifically.
Additionally, apps like AskPCOS and PCOS Challenge offer valuable resources to enrich doctor-patient discussions, empowering women seeking accurate diagnosis and care.
how to prevent or manage PCOS?
Primarily, it's crucial to understand that your dietary habits and lifestyle significantly impact the prevention and management of Polycystic Ovary Syndrome (PCOS). According to the National Institute of Health , a well-rounded diet low in processed foods and rich in whole foods is an effective strategy against PCOS. In fact, a diet that limits sugar and refined carbohydrates can help maintain insulin levels, which are crucial in the context of PCOS.
Physical activity also plays a quintessential role. A study indicated by The National Institute of Diabetes and Digestive and Kidney Diseases states that workouts can enhance insulin sensitivity, help manage weight, and balance hormone levels—all critical aspects in managing PCOS.
Finally, it's important to take stress management seriously. Engaging in mindfulness activities such as meditation and yoga, combined with adequate sleep, can combat both inflammation and hormone imbalance, subsequently easing the symptoms of PCOS.
The Centers for Disease Control and Prevention have estimated that implementing these changes can considerably reduce the influence of PCOS on your well-being, thus promoting your overall health.
so is pcos really on the rise?
Dr Cree confirms that cases are on the rise, according to The 2023 Endocrine Society International meeting.
“Another determinant can be there is more awareness as to clinical signs and symptoms and appropriate workups in countries where PCOS was not so readily diagnosed [in the past] due to a lack of resources,” Dr Grover shares. So enhanced awareness of the condition's signs and improved diagnostic resources in some regions are contributing to the uptick in diagnoses. The rise in awareness is empowering women to advocate for their health.
Dr Elisabet Stener-Victorin, a professor and principal investigator of the research group Reproductive Endocrinology and Metabolism in the department of physiology and pharmacology at Stockholm’s Karolinska Institutet, has been studying PCOS since 1995 and underscores the need for increased funding in PCOS research, stating that current funding levels are insufficient. By spotlighting PCOS in discussions and raising awareness, they hope to attract more funding and improve the quality of research on the condition.
the bottom line
Ultimately, the true impact and pervasiveness of PCOS may indeed be increasing, but it's essential to consider that better diagnosis and wider awareness of the condition may contribute to these statistics. Despite this, it's undeniable that PCOS presents a substantial health challenge, with far-reaching consequences for those affected.
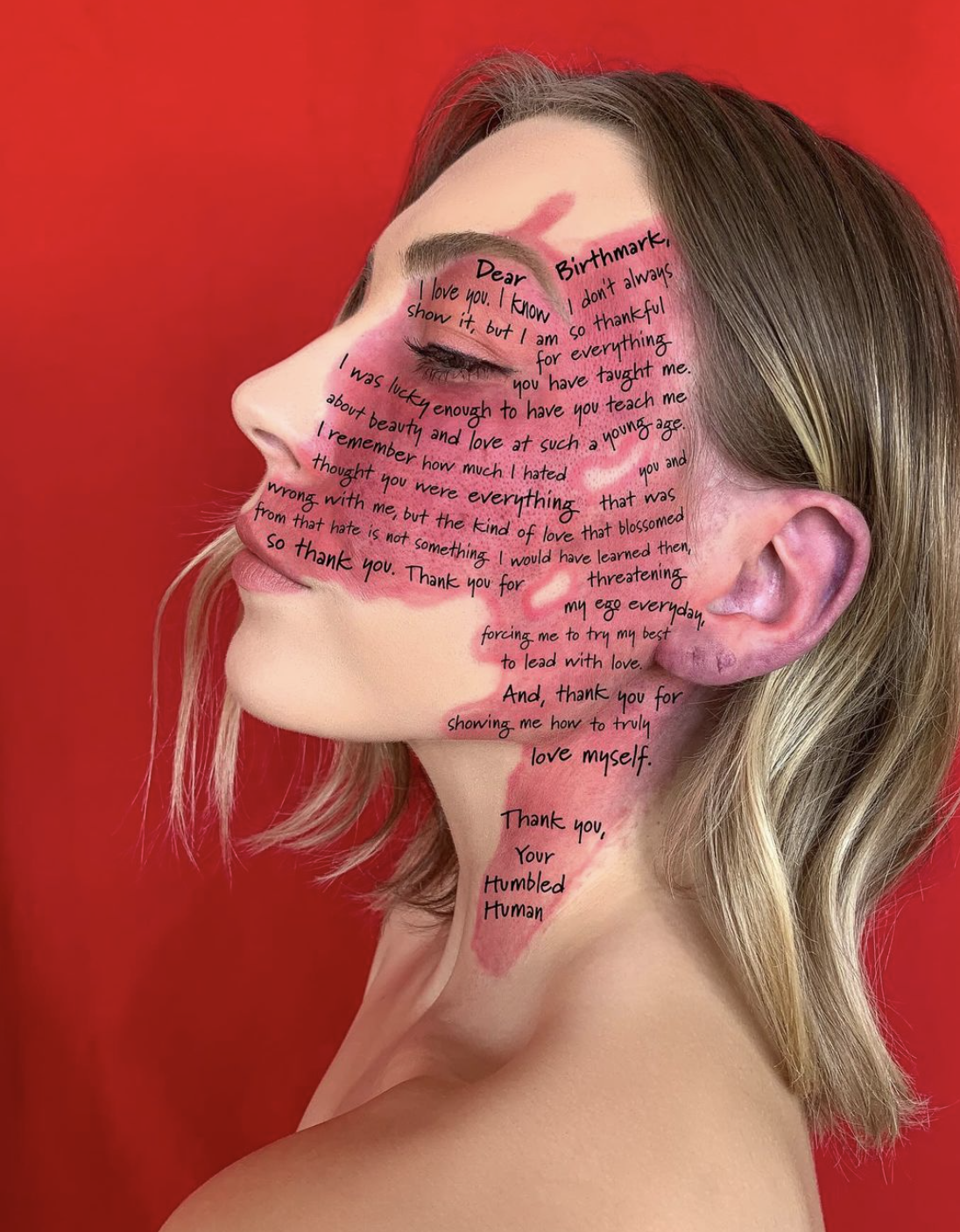
However, hope lies in the numerous treatments available and the power of educated choices. If you think you may have PCOS, reach out to a healthcare professional, take control of your health and remember - you're not alone. Together, we can increase understanding, improve management, and continue the ongoing body living approach to healing PCOS.